Where we stand with COVID-19 now
 As we come to the end of the Public Health Emergency on May 11th, I thought that it might be time to summarize where things stand with COVID-19 as of May 1, 2023.
As we come to the end of the Public Health Emergency on May 11th, I thought that it might be time to summarize where things stand with COVID-19 as of May 1, 2023.
A Look at the Numbers:
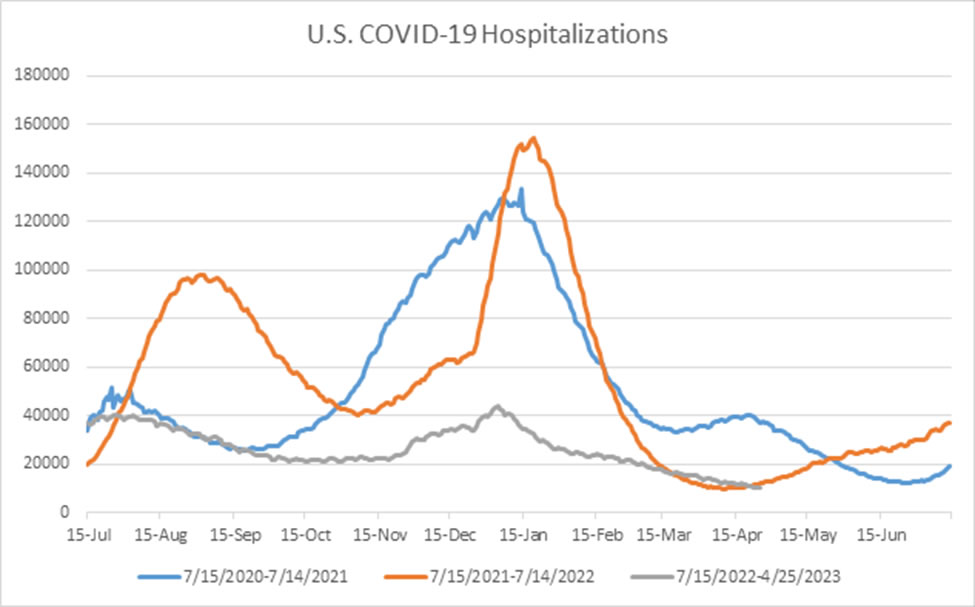
Sometimes it helps to remember where we have been. In the winter of 2020-2021, as we were just beginning to roll out the first COVID-19 vaccines, we reached a peak in the U.S. of over 133,000 patients hospitalized with COVID-19 on January 14, 2021, with close to 70% of ICU beds occupied by COVID-19 patients around that time. A year later, during the initial wave of the Omicron variant, hospitalizations in the U.S. rose to a peak of close to 155,000 patients hospitalized with COVID-19 on January 19, 2022, with around 64% of ICU beds occupied by COVID-19 patients at that time.
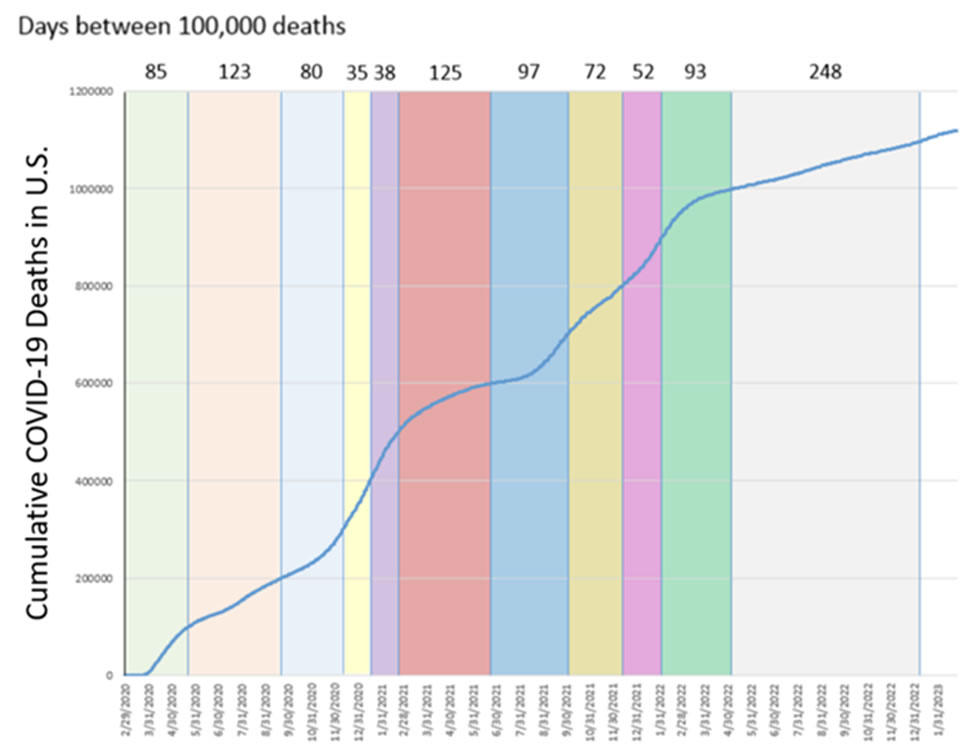
This year, hospitalizations peaked at 42,000-43,000 in the first week of January, a little over 72% lower than the year prior, with only 11% of ICU beds occupied by COVID-19 patients. At the peak of the 2020-2021 winter, it took only 5 weeks for 100,000 cumulative COVID-19 deaths in the U.S. By the peak of the 2021-2022 winter, it took 8 weeks for 100,000 cumulative deaths in the U.S. After reaching 1,000,000 deaths in May 2022, it took 248 days to reach 1.1 million deaths. This is not to minimize the over 1.1 million reported deaths from COVID-19 in the U.S., but this trend is very encouraging.
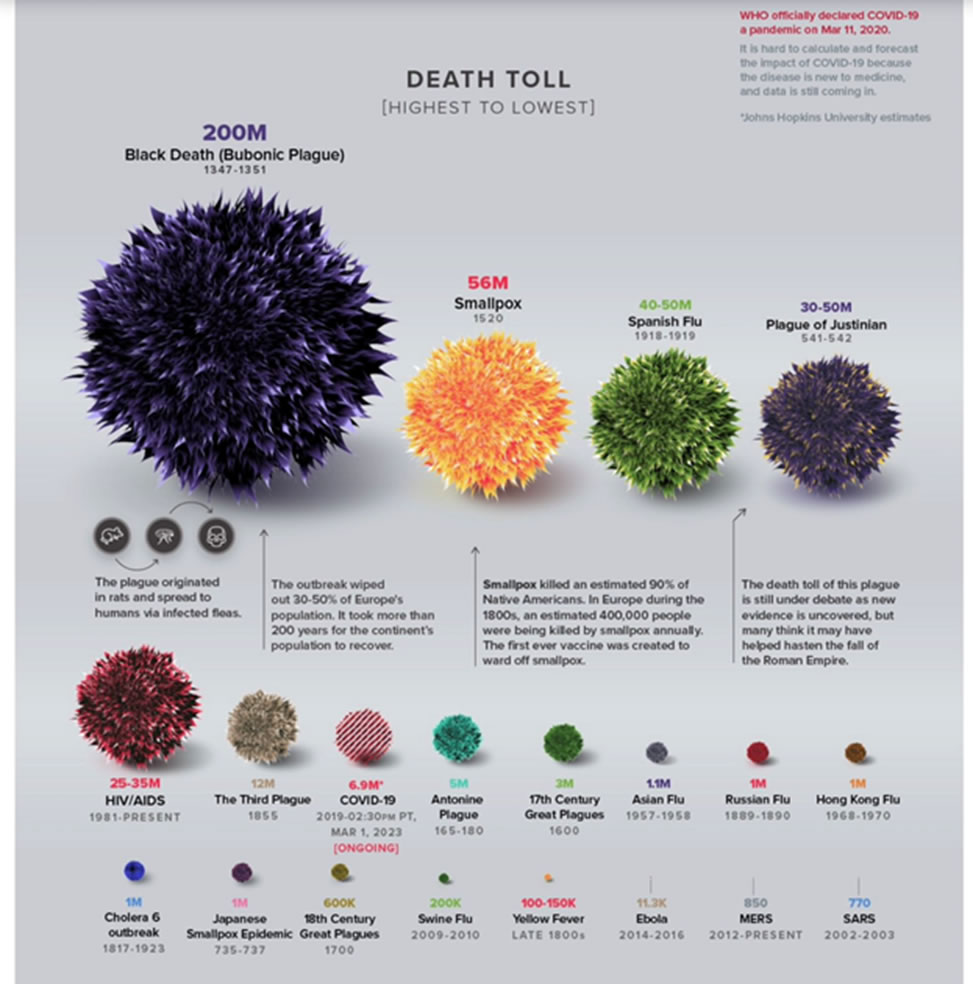
Worldwide, there have been 6.9 million COVID-19 deaths officially reported, with an estimate that true death toll is closer to 22 million. The pandemic’s true death toll | The Economist Here is a visualization compared with other pandemics:
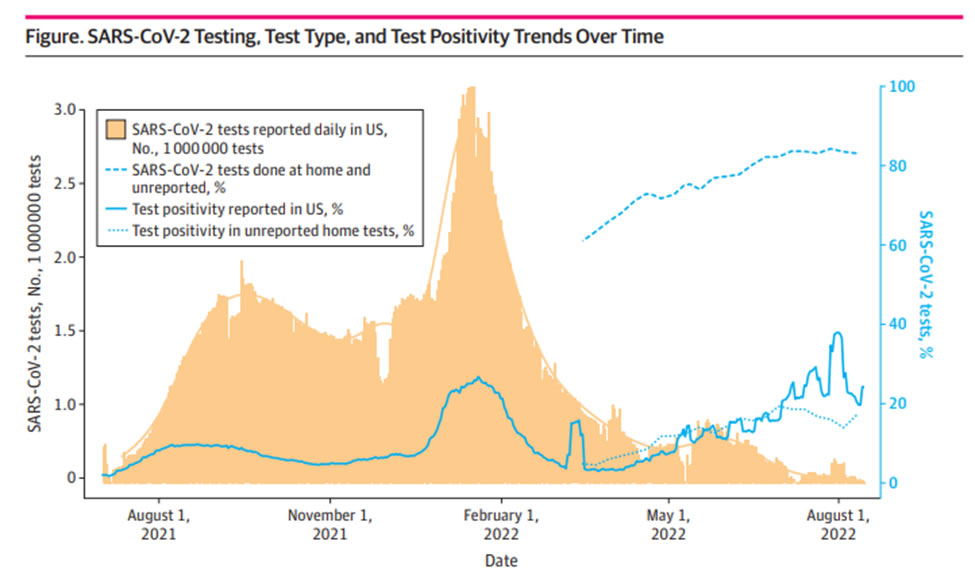
Based on the estimate that 80% of COVID-19 testing is now done at home, with a positivity rate tracking close to PCR testing data, a back of the envelope calculation is that there were close to 4.6 million tests done in the past week, and over 239,000 new cases (5.2% of those who tested). If 80% of tests are done at home and not reported, ~13 per 10,000 tested positive in the past week in the United States, down from ~2 per 1,000 at the start of April 2023, and 7 per 1,000 in late December 2022/early January 2023.
To compare, 7 out of every 100 people in the U.S. were reported as testing positive for COVID-19 over a 6 week period from December 2021-January 2022 (early Omicron), and this does not include tests done at home and unreported. Unreported SARS-CoV-2 Home Testing and Test Positivity | Infectious Diseases | JAMA Network Open | JAMA Network
Over the past month, there were an average of 12,911 hospital admissions per week with COVID-19 and an average of 1,342 deaths per week attributed to COVID-19. Around 5% are hospitalized with (although not necessarily for) COVID-19. Mortality rate is down to 0.5-0.6%. At the population level last week in the United States, there was a 3 in 100,000 chance of being hospitalized with COVID-19, and a 4 in 1,000,000 chance of dying from COVID-19. These were the risks in a single week.
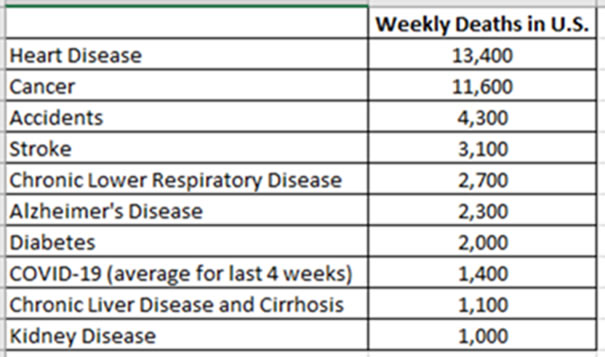
While COVID-19 remained the third leading cause of death in the United States in 2022, due to the early Omicron period, it is now down to the 8th leading cause of death in the past month:
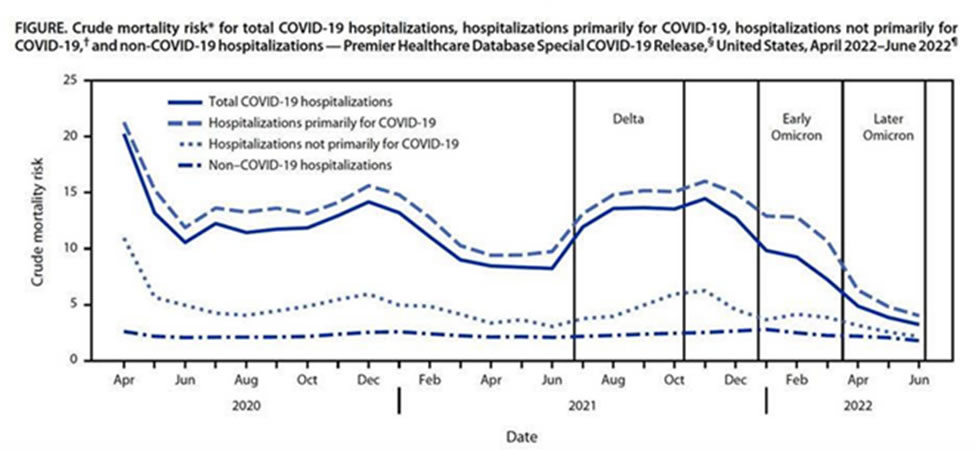
Thankfully, the mortality associated with COVID-19 among those who are hospitalized has continued to decline with newer variants, increasing immunity, and better therapies.
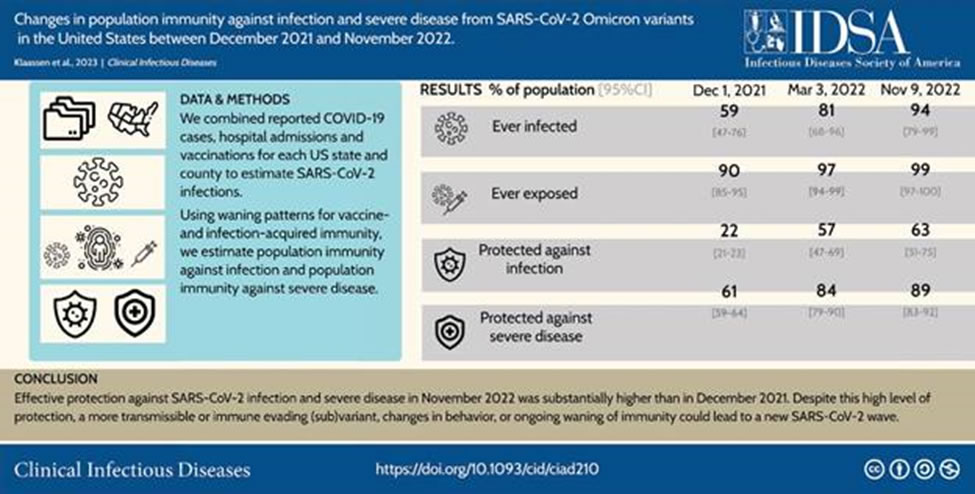
This population immunity was described nicely in a recent paper. Changes in population immunity against infection and severe disease from SARS-CoV-2 Omicron variants in the United States between December 2021 and November 2022 | Clinical Infectious Diseases | Oxford Academic (oup.com)
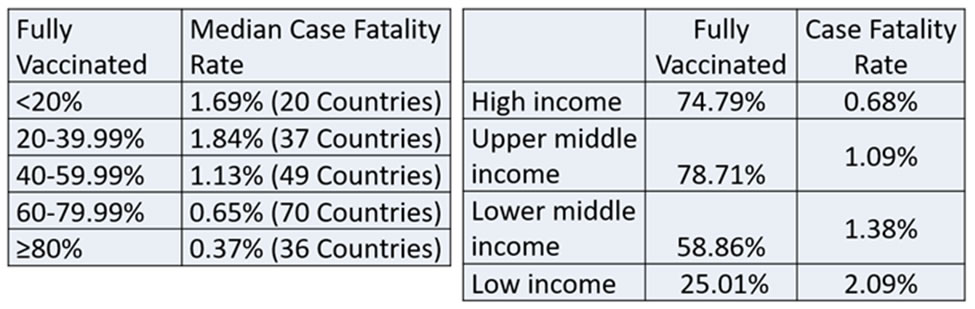
For the 212 countries reporting data on vaccination rates and case fatality rates, high vaccination rates predict lower case fatality rates, and vaccine equity remains a large problem. Data pulled from https://ourworldindata.org.
The lasting impact of long COVID also remains unknown. In June 2022, it was estimated that 7.3% of the U.S. adult population (18 million people) reported experiencing long-COVID, with 1.8% (4.6 million) having day-to-day activities impacted “a lot.” The prevalence was reported as 50% less in those who had been boosted at least once. Epidemiology of Long COVID in US Adults | Clinical Infectious Diseases | Oxford Academic (oup.com)
Those with no known COVID-19 infection had a 20% decrease per month in neutralizing antibodies after vaccine dose #2 but a sustained level of neutralizing antibodies out to 250 days after dose #3. This is part of the reasoning for why the COVID-19 vaccine is expected to be an annual vaccine, much like the influenza vaccine. Impact of Severe Acute Respiratory Syndrome Coronavirus 2 Vaccination and Infection on Neutralizing Antibodies: A Nation-wide Cross-sectional Analysis | The Journal of Infectious Diseases | Oxford Academic (oup.com)
Changing Policies in Healthcare:
Masks –
- I want to start by saying that the dialogue around masks has become quite heated. Change can be hard, and it is important to acknowledge the impact that this pandemic has had on so many in our communities.
- In January 2023, there was a lot of press about this Cochrane Review: Physical interventions to interrupt or reduce the spread of respiratory viruses - PMC (nih.gov). It is important to acknowledge that there has been a high risk of bias in the trials evaluating the effect of masks, variation in what has been measured in terms of transmission metrics, and relatively low adherence in many community settings limiting conclusions.
- Overall, the efficacy of masks for preventing spread of COVID-19 is estimated to be 10-45%, and they were a critical part of in our response to the pandemic. What Worked Against Covid: Masks, Closures and Vaccines - WSJ, Opinion | Here’s Why the Science Is Clear That Masks Work - The New York Times (nytimes.com)
- Using an efficacy of 10-45%, masks may have prevented 550k-2.5 million U.S. cases per week in January 2022.
- Similarly, while “lock-downs” are no longer in effect, and no longer make sense, they were important earlier in the pandemic. Without indoor closures, it is estimated that COVID-19 deaths in the U.S. would have been twice as high in 2020 (700k dead in year 1).
- “Until vaccines were available, [the countries that were most successful in containing COVID-19] used masking and selective closures (based on accurate, real-time data) just before a wave hit. They then reopened as soon as possible, quickly vaccinating those at highest risk and keeping vaccinations up to date.”
- Community masking policies had the greatest impact when COVID-19 risk was high and when vaccine availability was low. Condition-Dependent and Dynamic Impacts of Indoor Masking Policies for COVID-19 Mitigation: A Nationwide, Interrupted Time-Series Analysis | Clinical Infectious Diseases | Oxford Academic (oup.com)
- Most are aware that the CDC has had two sets of maps: 1. Community Level maps, with masks recommended in the community when the Community Level for your area was high (currently 12 counties in the U.S.) [CDC COVID Data Tracker: County View] AND 2. Transmission Level maps to determine infection control interventions in healthcare facilities [CDC COVID Data Tracker: County View]. Since September 2022, CDC guidance has said: “When SARS-CoV-2 Community Transmission levels are not high, healthcare facilities could choose not to require universal source control.” Infection Control: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) | CDC. Currently, ~80% of U.S. counties no longer have high community transmission, and many U.S. hospitals are moving away from universal masking based on their local risk.
- Some of the data are as follows:
- Data recently presented at the European Congress of Clinical Microbiology & Infectious Diseases evaluated the impact of universal masking in the UK after the NHS removed a healthcare mask mandate in June 2022. Comparing wards that continued universal masking with those that did not, there was no observed increase in hospital-acquired SARS-CoV-2 infections. While data from the middle of a traditional respiratory virus season would add to this analysis, they did have data during a period of increased transmission in the community. Requirement to wear masks in hospitals may have had little impact on COVID-19 transmission during omicron wave (medicalxpress.com)
- Looking at sources of exposure among health care workers, this has been more likely to have occurred in the community (Sources of exposure and risk among employees infected with severe acute respiratory coronavirus virus 2 (SARS-CoV-2) in a large, urban, tertiary-care hospital in the United States - PubMed (nih.gov)).
- In addition, the seroprevalence of SARS-CoV-2 among employees was not significantly different among those who provided direct patient care and those who did not. … Employees who reported direct personal contact with COVID-19-positive persons outside work were more likely to have SARS-CoV-2 antibodies. (Seroprevalence of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection among Veterans Affairs healthcare system employees suggests higher risk of infection when exposed to SARS-CoV-2 outside the work environment - PubMed (nih.gov)).
- A group of hospital epidemiologists (including myself) wrote an opinion piece for the Annals of Internal Medicine concluding that, “The time has come to deimplement policies that are not appropriate for an endemic pathogen when the expected benefits of such policies are low. Universal masking in health care is a policy whose time has come and gone ... for now.” Universal Masking in Health Care Settings: A Pandemic Strategy Whose Time Has Come and Gone, For Now | Annals of Internal Medicine (acpjournals.org)
- I recognize that there are differing opinions on this topic, and I particularly liked this Pro/Con: SHEA Podcasts: To Mask or Not to Mask as Part of Standard Precautions? on Apple Podcasts
- Dr. Shenoy summarized some of our points about the downsides of universal masking as follows: “Masking impedes communication. That barrier is not equally distributed across patent populations. It’s more of an impact in patients for whom English is not their preferred language, those who are hard of hearing, and those who rely on lip reading and non-verbal cues. There is also good evidence that the increase in listening effort that is required when masks are used in clinical encounters is associated with increased cognitive load not only for patients but also for clinicians. In addition, masks obscure facial expression which can contribute to feelings of isolation and negatively impact human connection, trust, and perception of empathy.” The references are in our Annals paper.
- There will be times when universal masking may be indicated in the future. “Future pandemics or significant localized outbreaks may justify more widespread or targeted masking policies, respectively, as part of a bundled response.”
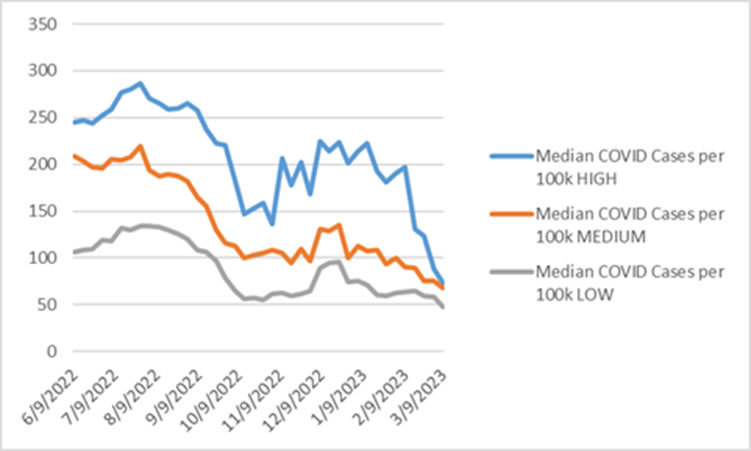
- Some are asking how we will track COVID-19 activity now that the CDC will no longer be updating their maps with the end of the public health emergency. Much like we do for other endemic viruses, we will continue to track local testing trends and hospitalizations closely. The best measure discriminating high, medium, and low community levels is COVID-19 admissions per 100,000 in the past 7 days. On the other hand, new cases per 100,000 in the past 7 days has declined significantly across all community levels.
Asymptomatic Screening
- Hospitals have moved away from asymptomatic admission screening at different times over the past year. Stanford Health presented data at the recent Spring Conference of the Society for Healthcare Epidemiology of America showing that only 1 in 20 asymptomatic patients testing (+) for COVID-19 by SARS-CoV-2 PCR on admission had ongoing viral replication (infectivity).
- Data from Japan also showed that there was “no increasing trend in nosocomial clusters…observed during community-based surges before and after discontinuation” of universal pre-admission screening. Discontinuation of admission screening for coronavirus disease 2019 (COVID-19) and the impact on in-hospital clusters of COVID-19: Experience at a tertiary-care center | Infection Control & Hospital Epidemiology | Cambridge Core
- The Cleveland VA Medical Center also reported that, “Asymptomatic but noninfectious patients experienced a variety of adverse effects, including delays in care and unnecessary isolation and treatment.” More harm than good? Potential benefits and unintended consequences associated with screening asymptomatic hospital admissions for severe acute respiratory syndrome coronavirus 2 | Infection Control & Hospital Epidemiology | Cambridge Core
Updated Vaccine Recommendations:
This is a question that I have received a lot recently. Per updates made on April 19, 2023 (CDC simplifies COVID-19 vaccine recommendations, allows older adults and immunocompromised adults to get second dose of the updated vaccine | CDC Online Newsroom | CDC):
- CDC’s new recommendations allow an additional updated (bivalent) vaccine dose for adults ages 65 years and older and additional doses for people who are immunocompromised. This allows more flexibility for healthcare providers to administer additional doses to immunocompromised patients as needed.
- Monovalent (original) mRNA COVID-19 vaccines will no longer be recommended for use in the United States.
- CDC recommends that everyone ages 6 years and older receive an updated (bivalent) mRNA COVID-19 vaccine, regardless of whether they previously completed their (monovalent) primary series.
- Individuals ages 6 years and older who have already received an updated mRNA vaccine do not need to take any action unless they are 65 years or older or immunocompromised.
- Expectation that all will be recommended to get an updated booster in Fall 2023.
Lessons Learned:
If you are interested in reading about the experience of infectious diseases physicians in battling this pandemic over the past three years, I recommend this paper that just came out on April 27, 2023: How Infectious Disease Experts Impacted the Coronavirus Disease 2019 (COVID-19) Response: Lessons From the Front Lines | Clinical Infectious Diseases | Oxford Academic (oup.com).
